Abstract

Introduction
Salvage therapy with high dose chemotherapy and hematopoietic stem cell transplant (HDC/SCT) is recommended for eligible patients (pts) with relapsed/refractory (R/R) PTCL. The majority of studies have reported outcomes from the point of SCT, with limited data available in those where there is an 'intention to transplant' (ITT). We evaluated the outcomes of R/R PTCL from the time of first relapse/progression in patients intended for SCT.
Methods
The BC Cancer Lymphoid Cancer Database was reviewed and pts ≥ 18 years with relapsed or refractory nodal PTCLs (R/R PTCLs) including systemic anaplastic large cell lymphoma (ALCL), angioimmunoblastic T-cell lymphoma (AITL) and PTCL-not otherwise specified (PTCL-NOS). ITT was assessed from documentation in clinical records. Outcomes were assessed from the time of first relapse or progressive disease (PD) and from the time of SCT.
Results
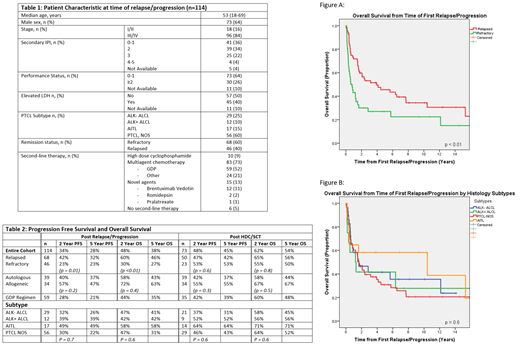
A total of 114 pts with ITT R/R PTCL were identified (original PTCL diagnosis between 1981-2020, 85% > 2000). 68 (60%) had refractory disease (PD on primary therapy or progression < 3 months (m) from treatment completion) and 46 (40%) had relapsed disease. Those with refractory disease were more likely to have secondary IPI (sIPI) score of ≥ 2 (79% vs. 52%, p = 0.01), poor performance status (PS) >2 (46% vs. 19%, p = 0.003) or advanced stage disease (94% vs. 78%, p = 0.02) at the time of first relapse/progression. Most pts had received anthracycline based chemotherapy as part of first line treatment (94%) including 3 pts who received consolidative auto-.
For second-line therapy, the majority received multi-agent chemotherapy (n = 83, 73%) with GDP (gemcitabine, dexamethasone and cisplatin) the most commonly used regimen (n = 59, 52%); 10 pts received single agent high dose cyclophosphamide in the earlier era; and 15 pts (13%) received novel agents (brentuximab vedotin [BV] = 12: ALK-negative ALCL [8], ALK-positive ALCL [3], AITL [1]; romidepsin = 2: AITL [1], PTCL-NOS [1]; pralatrexate = 1: PTCL-NOS). 6 pts did not receive any intervening salvage and proceeded directly to HDC/SCT (n=3 auto; n=3 allo). (Table 1) For those that received systemic therapy, the overall response rate (ORR) to second-line therapy was 61% (24% CR; 37% PR). The ORR to GDP was 61% (17% CR; 44% PR) with higher responses observed in relapsed versus refractory pts (81% vs. 41%, p=0.002). The ORR to BV was 75% (25% CR; 50% PR).
Ultimately, 73 R/R PTCL pts (63%) received HDC/SCT (50/68 [74%] relapsed; 23/46 [50%] refractory) of which 39 pts, underwent auto-SCT and 34 pts had an allo-SCT (myeloablative n=25, 74%). AITL pts were more likely to receive an allo-SCT than other subtypes (71% vs. 41%, p = 0.04). Those who underwent allo-SCT were younger (median age of 47 y) and more likely to have refractory disease (50% vs. 16%, p = 0.001) compared to those that underwent auto-SCT. PD was the main reason for not proceeding to HDC/SCT (76%) and for the remainder the reason was, pts choice (12%), chemotherapy toxicity (5%), poor PS/comorbidities (5%) and lack of donor (2%). In total, 50/67 (75%) received only second-line therapy prior to SCT, most commonly GDP (23/50, 46%). 17/67(25%) required additional third-line therapy, including novel agents in 9 cases prior to SCT.
The median follow up for living pts from time of relapse/progression was 6.8 years (y) (range 0.3 to 30.7). The 5 y progression free survival (PFS) and overall survival (OS) from the time of first relapse/progression for the ITT population was 28% and 38% respectively, and was inferior in those with refractory vs relapsed disease (5 y PFS 23% vs 32%, p=0.01; 5 y OS 27% vs 46% p<0.01). (Fig. A) The 5 y PFS from auto and allo-SCT were 37% and 55% (p = 0.3) and 5 y OS was 44% and 67% (p = 0.5) respectively. Considering pts who received GDP(n=59) as second-line therapy, the 5 y PFS and OS was 21% and 35% from first relapse/progression, and 39% and 48% from SCT (auto n=21; allo n=14). Outcome was similar amongst the PTCL subtypes. (Fig. B)
Conclusion
Overall, outcomes in the ITT R/R PTCLs remain suboptimal with long-term survival in about only 1/3 of pts, but over half are alive at 5 years if they are able to receive a SCT, with similar results in the modern era using second-line GDP chemotherapy. A third line of therapy may be a successful bridge to SCT and novel agents should be considered in this setting. Despite higher proportion of refractory pts, results are encouraging for pts able to receive an allo-SCT.
Scott: AstraZeneca: Consultancy; Celgene: Consultancy; Incyte: Consultancy; Janssen: Consultancy, Research Funding; NanoString Technologies: Patents & Royalties: Patent describing measuring the proliferation signature in MCL using gene expression profiling.; Abbvie: Consultancy; BC Cancer: Patents & Royalties: Patent describing assigning DLBCL COO by gene expression profiling--licensed to NanoString Technologies. Patent describing measuring the proliferation signature in MCL using gene expression profiling. ; Rich/Genentech: Research Funding. Villa: Janssen: Honoraria; Roche: Honoraria; Lundbeck: Honoraria; Celgene: Honoraria; Seattle Genetics: Honoraria; AbbVie: Honoraria; AstraZeneca: Honoraria; Gilead: Honoraria; NanoString Technologies: Honoraria. Gerrie: AbbVie: Honoraria, Research Funding; Roche: Research Funding; Astrazeneca: Honoraria, Research Funding; Sandoz: Honoraria; Janssen: Honoraria, Research Funding. Slack: Seagen: Consultancy, Honoraria. Song: Bristol Myers Squibb: Honoraria; Janssen: Honoraria, Research Funding; Sanofi: Honoraria; Takeda: Consultancy, Honoraria; Kite, a Gilead Company: Honoraria; Celgene: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria; GlaxoSmithKline: Honoraria. Sehn: Novartis: Consultancy; Genmab: Consultancy; Debiopharm: Consultancy. Savage: BMS: Consultancy, Honoraria, Other: Institutional clinical trial funding; Roche: Research Funding; Servier: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria; Astra-Zeneca: Consultancy, Honoraria; Takeda: Other: Institutional clinical trial funding; Merck: Consultancy, Honoraria, Other: Institutional clinical trial funding; Seattle Genetics: Consultancy, Honoraria; Beigene: Other: Institutional clinical trial funding; Genentech: Research Funding.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal